Thrombocytopenia
Thrombocytopenia is a condition characterized by an abnormally low number of platelets in the blood. Platelets, or thrombocytes, are small blood cell fragments essential for normal blood clotting.
Signs and Symptoms
The severity of symptoms in thrombocytopenia can vary widely based on the underlying cause and the degree of platelet reduction. Common signs and symptoms include:
· Petechiae: Small, red or purple spots on the skin caused by bleeding.
· Purpura: Larger purple or red bruises that can occur with minimal or no trauma.
· Prolonged bleeding: Bleeding that does not stop easily, including frequent nosebleeds or bleeding gums.
· Menorrhagia: Heavier than normal menstrual bleeding.
· Hematuria: Blood in the urine.
· Hematochezia: Blood in the stool.
· Fatigue: General tiredness and weakness due to blood loss.
· Splenomegaly: Enlarged spleen, which can be felt in the abdomen.
Pathophysiology
The mechanisms leading to thrombocytopenia can be classified into three main categories:
Decreased Platelet Production:
· Bone marrow disorders (e.g., leukemia, aplastic anemia, myelodysplastic syndromes)
· Viral infections (e.g., HIV, hepatitis C)
· Chemotherapy or radiation therapy
· Vitamin deficiencies (e.g., B12 or folate)
Increased Platelet Destruction:
· Immune thrombocytopenic purpura (ITP)
· Drug-induced thrombocytopenia (e.g., heparin-induced thrombocytopenia)
· Autoimmune diseases (e.g., systemic lupus erythematosus)
· Infections (e.g., sepsis, dengue fever)
· Disseminated intravascular coagulation (DIC)
Increased Platelet Sequestration:
· Splenomegaly (e.g., due to liver disease, lymphomas)
Dilutional Thrombocytopenia:
· Massive blood transfusions which can dilute platelets.
Diagnosis
The diagnosis of thrombocytopenia involves several steps:
· Medical History and Physical Examination: Assessment for symptoms, history of bleeding, family history, and any potential drug use or exposure to toxins.
· Complete Blood Count (CBC): To measure the platelet count and evaluate other blood cells.
· Peripheral Blood Smear: To examine the appearance of platelets and other blood cells.
· Bone Marrow Biopsy: If bone marrow production issues are suspected.
· Additional Tests: Depending on suspected causes, additional tests may include liver function tests, viral serologies, autoimmune markers, and imaging studies (e.g., ultrasound or CT scan of the spleen).
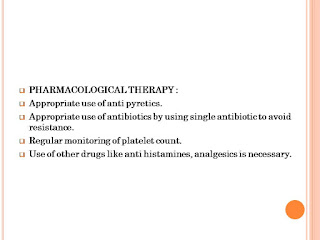
Management
The management of thrombocytopenia depends on its cause, severity, and the presence of symptoms. General strategies include:
Addressing Underlying Cause:
· Treating infections or discontinuing causative drugs.
· Managing underlying diseases (e.g., liver disease, autoimmune conditions).
· Bone marrow stimulants for production issues.
Supportive Care:
· Platelet transfusions in cases of severe thrombocytopenia or active bleeding.
· Avoidance of activities that could cause bleeding or bruising.
· Use of medications to reduce bleeding risk, such as antifibrinolytic agents.
Specific Treatments:
· Immune Thrombocytopenic Purpura (ITP): Corticosteroids, intravenous immunoglobulin (IVIG), rituximab, or splenectomy.
· Heparin-Induced Thrombocytopenia (HIT): Discontinuation of heparin and use of alternative anticoagulants.
· Aplastic Anemia: Immunosuppressive therapy or hematopoietic stem cell transplantation.
· TTP/HUS: Plasma exchange and immunosuppressive therapy.
Long-term Monitoring:
· Regular follow-ups to monitor platelet counts and adjust treatments as needed.
· Management of any chronic conditions contributing to thrombocytopenia.
In summary, thrombocytopenia requires a thorough diagnostic evaluation to determine the underlying cause and appropriate management strategy. Timely intervention can effectively manage the condition and prevent complications.
This is a case presentation on thrombocytopenia.
In any given case 1st we have to look at the major problems that a patient is facing and to make a plan to resolve them
¢ PROBLEM 1 (FEVER): Fever is when a human's body temperature goes above the normal range of 36–37° Centigrade (98–100° Fahrenheit). It is a common medical sign. Other terms for a fever include pyrexia and controlled hyperthermia.
¢ PROBLEM 2 (HEADACHE): A headache can be a sign of stress or emotional distress, or it can result from a medical disorder, such as migraine or high blood pressure, anxiety, or depression. It can lead to other problems.
¢ PROBLEM 3 (DRY COUGH): Cough is a reflex action that clears your airway of irritants and mucus. A nonproductive cough, also known as a dry cough, doesn’t produce phlegm or mucus.













.webp)

0 Comments